We all do this every single day. We measure target many of our interventions in the critically ill patients to blood pressure. Whether it’s fluids, vasopressors, or blood pressure lowering agents, we obsess over these parameters. We feel warm and fuzzy if it’s okay. But are we using the right tool to find out these numbers?
I’ve always harped on arterial lines, although invasive, being the most reliable method of evaluating the blood pressure in our patients. If someone is critically ill on jet fuel, they’re getting an a-line. This is a fun study where they compared the oscillometric BP cuffs to a-lines in 736 patients.
When you look at the mean differences they obtained, the numbers weren’t too bad.
Systolic: 0.8mmHg
Diastolic: -2.9mmHg
Mean Arterial pressure: -1mmHg
This wouldn’t drive any of us crazy, right? We’d be cool with these differences if it avoids invasive (painful) interventions on our patients. But wait, there’s more. There was a large amount of variability which could lead to additional interventions.
Systolic: ± 15.7mmHg
Diastolic: ± 11mmHg
MAP: ± 10.2mmHg
The article goes as far as to say that BP cuffs would not pass the Association for the Advancement of Medical Instrumentation standards. There’s no data as to how this changes outcomes.
This was a post hoc analysis (after the fact). This shouldn’t be too challenging to accomplish a prospective study looking at this in our critically ill patients. We have many patients who have a BP cuffs and an a-line in place. Why not just record cuff pressures every 15 minutes and obtain some data? Obviously it’s more complicated than that.
A hat tip to the authors.
T. Kaufmann, E.G.M. Cox, R. Wiersema, et al., Non-invasive oscillometric versus invasive arterial blood pressure measurements in critically ill patients: A post hoc analysis of a prospective observational study, Journal of Critical Care(2019)
Link to full article (not free)
Although great care has been taken to ensure that the information in this post is accurate, eddyjoemd, LLC shall not be held responsible or in any way liable for the continued accuracy of the information, or for any errors, omissions or inaccuracies, or for any consequences arising therefrom.
My passion is taking care of the critically ill using evidence-based medicine and teaching others how to do the same.
Links to my other projects
Showing posts with label blood pressure. Show all posts
Showing posts with label blood pressure. Show all posts
Sunday, February 23, 2020
Saturday, February 22, 2020
Oscillometric devices vs Arterial lines. New data.
Why is it important to stay up to date? There’s a pendulum in medicine but there’s a time when the pendulum swing is going to bite you in the butt and you’re going to be wrong. Seems like I’m wrong.
I have an extremely popular post and YouTube video regarding how oscillometric devices are correct with regards to their MAP but not their SBP and DBP. I hadn’t found any studies to validate how the SBP and DBP applied. Now we have data. And I may have to eat my words. I’m cool with that, though. This study was published earlier today. I cannot get my hands on it to take it apart, but the data is compelling. They did some fancy statistics that I can’t admit to understand including Bland-Altman and error grid analyses. Although the averages seem to be close, the variations are as follows:
SAP 0.8 mmHg (±15.7 mmHg, −30.2 to 31.7 mmHg)
DAP −2.9 mmHg (±11.0 mmHg, −24.5 to 18.6 mmHg)
MAP −1.0 mmHg (±10.2 mmHg, −21.0 to 18.9 mmHg)
The interesting part is that the ICU is a world of details and although the differences were small. The variation between the two, radial arterial line and oscillometric cuff, was enough though to cause additional treatment changes in more than 20% of patients.
I despise reading abstracts and coming to conclusions but at this point I have no choice. Maybe tomorrow I’ll be able to take this apart entirely.
Link to abstract
EJ
Kaufmann T, Cox EGM, Wiersema R, et al. Non-invasive oscillometric versus invasive arterial blood pressure measurements in critically ill patients: A post hoc analysis of a prospective observational study [published online ahead of print, 2020 Feb 22]. J Crit Care. 2020;57:118–123. doi:10.1016/j.jcrc.2020.02.013
Although great care has been taken to ensure that the information in this post is accurate, eddyjoemd, LLC shall not be held responsible or in any way liable for the continued accuracy of the information, or for any errors, omissions or inaccuracies, or for any consequences arising therefrom.
I have an extremely popular post and YouTube video regarding how oscillometric devices are correct with regards to their MAP but not their SBP and DBP. I hadn’t found any studies to validate how the SBP and DBP applied. Now we have data. And I may have to eat my words. I’m cool with that, though. This study was published earlier today. I cannot get my hands on it to take it apart, but the data is compelling. They did some fancy statistics that I can’t admit to understand including Bland-Altman and error grid analyses. Although the averages seem to be close, the variations are as follows:
SAP 0.8 mmHg (±15.7 mmHg, −30.2 to 31.7 mmHg)
DAP −2.9 mmHg (±11.0 mmHg, −24.5 to 18.6 mmHg)
MAP −1.0 mmHg (±10.2 mmHg, −21.0 to 18.9 mmHg)
The interesting part is that the ICU is a world of details and although the differences were small. The variation between the two, radial arterial line and oscillometric cuff, was enough though to cause additional treatment changes in more than 20% of patients.
I despise reading abstracts and coming to conclusions but at this point I have no choice. Maybe tomorrow I’ll be able to take this apart entirely.
Link to abstract
EJ
Kaufmann T, Cox EGM, Wiersema R, et al. Non-invasive oscillometric versus invasive arterial blood pressure measurements in critically ill patients: A post hoc analysis of a prospective observational study [published online ahead of print, 2020 Feb 22]. J Crit Care. 2020;57:118–123. doi:10.1016/j.jcrc.2020.02.013
Although great care has been taken to ensure that the information in this post is accurate, eddyjoemd, LLC shall not be held responsible or in any way liable for the continued accuracy of the information, or for any errors, omissions or inaccuracies, or for any consequences arising therefrom.
Saturday, August 17, 2019
Blood Pressure Measurements in the ICU: Trust ONLY the MAP in Oscillometric Devices!

Link to Abstract
Link to Article
Full disclosure. I did not learn this until I was a fellow in Critical Care Medicine. It is not widely taught. Do not feel bad that you did not know this. All I ask is for your help to share this with others so we all speak the same language and do the best for our patients.
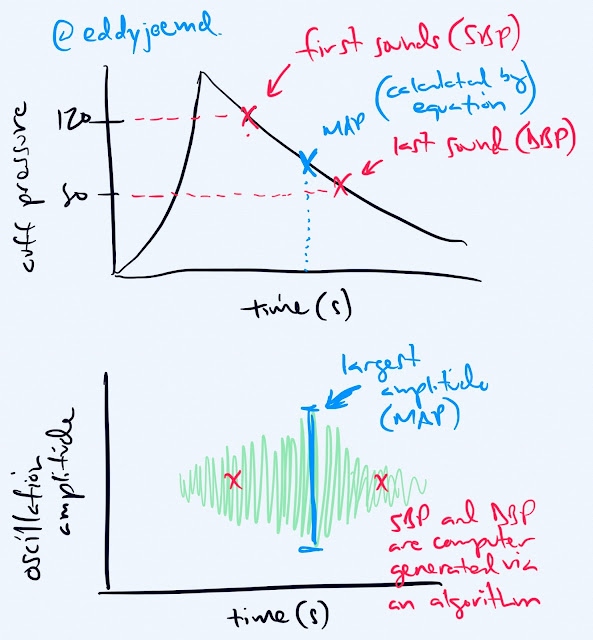
What are the normal sounds you hear with the "old fashioned"/auscultatory method of taking a patients blood pressure?
Those sounds define the systolic blood pressure and diastolic blood pressure respectively.
Then you do math and could calculate the mean arterial pressure (MAP) by using the formula of (2xDBP)+SBP/3 but there are a number of different ways to derive the MAP.
Does the BP cuff you have in the ICU, hospital or throughout the majority of doctor offices have ears? We if that's the case, you CANNOT assume that the SBP and DBP provided by these devices are exact.
How do oscillometric devices work?
The device measures the oscillations from the blood vessel wall during cuff deflation. The maximal oscillation point is the MAP. The device uses an algorithm that is proprietary to define the SBP and DBP. Those algorithms are closely kept secrets to the manufacturers.
Why is this important, well, BP is GOLD in the ICU world. My nurses titrate pressors based on MAP number, as the guidelines suggest, but I have too often seen nurses whipping out their phone calculating the MAP by hand as they feel that the numbers generated on the screen are inaccurate. Now, this occurred when I trained in community academic hospital, then ivory tower fancy pants hospital, and now in a community hospital which is why I feel writing this post is so important. We need to understand how our technology works!
It is known, however, that the MAP is the most important value generated by the device.
The study listed above noted that there was a significant difference between calculated MAP, i.e. the nurses/staff doing the calculation themselves, and the observed MAP (generated by the machine). They found that the generated MAP could either be lower or higher that the observed MAP. These differences were amplified even further when analyzed on individual patients rather than the cohorts. Would you feel comfortable treating your patients like this? I sure don't.
The authors discuss a trial where patients had their BP taken via oscillometric device in the OR vs. intraarterial and there was no statistically significant difference in the MAP. There was a difference in the SBP by 19mmHg, though. Could you imagine treating these patients based on an algorithm generated SBP? You'd be treating them (or not treating them) inappropriately!
Now, this post may seem like it's being directed at nurses, after all, you all are the main ones at the bedside, but we all need to get better. The docs needs to stop presenting patients to each other by referencing the SBP. Docs need to stop telling nurses to hit SBP goals for their pressors instead of MAPs.
Well, now you know how this all works and you won't make silly comments anymore. I hope I taught you something.
- EJ
Subscribe to:
Comments (Atom)
-
This is a topic better handled by Surgeons than myself but I haven't seen anyone do it. Here I go! @buckparker, you're invited to ch...
-
Not Just Oxygen? Mechanisms of Benefit from High-Flow Nasal Cannula in Hypoxemic Respiratory Failure. Link to Abstract Link to Image Goli...
-
Trying something new... stay tuned... -EJ