The article I'm referencing in this post is titled: An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy. It was published in the American Journal of Respiratory and Critical Care Medicine in June of 2019.
We see this every day in the intensive care unit. A patient with pneumonia sucking wind. Tachypenic. Slightly altered. Requiring a bunch of oxygen. Should we intubate them and place them on mechanical ventilation, or should we give them a shot and see if they fly on high flow nasal cannula? The data for pneumonia and using BiPAP isn't there so that's not an option. Side note, check the FLORALI trial which I posted on my site as it has some of the same researchers on the matter. I really really don't want to have to intubate the patient with all the risks and complications known to go with that unless it's really really needed. In a joking manner, we all think we're big shots and can call it just by seeing it. You know the type, I am the same way. I can tell a patient needs to be intubated as soon as I lay eyes on them. Big shot. Yep. This is true, or is it? We also know that delaying intubation is far worse for patient populations that just intubating them early on. What ends up happening is that once you finally go ahead and proceed with intubation after the patient has been developing more and more fatigue, you notice that you're in deep poop when the induction agents destroy your patients hemodynamics. Start bolusing fluids. Place a central line and start vasopressors. Death spiral ensues. If this hasn't happened to you in your career, you haven't been working long enough.
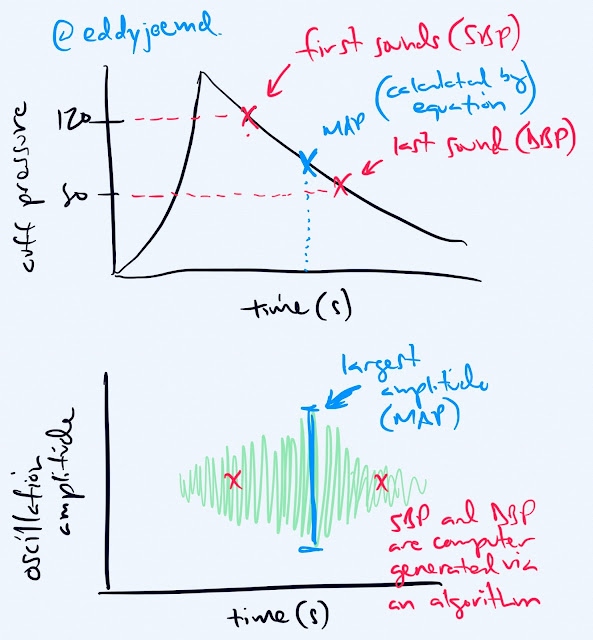
What if there was a tool to help us with this decision? Wouldn't that be great? How about a tool so simple that all you need is a pulse oximeter, a HFNC setup telling you the FiO2 being delivered to the patient, and a set of eyeballs to count a patients respiratory rate (because we all know that whatever device measures RR on the monitor is inaccurate and showing "apneic" more often than it should). Well, we're all in luck! These authors came up with the ROX index which is (SpO2/FiO2)/RR. SpO2 is the number you get from the pulse oximeter and it's on the monitor. It should be entered as a whole number. FiO2 is entered as a decimal. For example room air is 21% so 0.21. RR is, well, respiratory rate. Based on the data provided in this article, it should be a statistically significant prediction of whether your patient is going to be intubated or not. Hopefully the delay of mechanical ventilation we all are dreading should be avoided. This should also help you make the decision to just intubate the person before you leave your partner who is working the opposite shift with an airway dump, one of the worst kinds of dumps.
I am not going to go deep into the data of this study because this team knows what they are doing far better than I ever will and the truth is that the abstract here is a pretty darn good representation of what is within the bulk of the text. I am curious, however, of why the article was published in its "in press" format in December of 2018 and was not fully released until June 2019. So many people could have benefitted from it.
Also, a little tidbit that you may or may not have known. The journal where this was published, the American Journal of Respiratory and Critical Care Medicine is the high ranked journal for Critical Care Medicine based on Impact Factor. Don't know what Impact Factor is? You should definitely check it out because it evaluates the quality of the journal. That will keep you from making a mistake that I made where I showed my Program Director in residency an article from this small European journal something about atrial fibrillation and then he proceeded to make fun of me and showed me where to look up the actual data on afib, the American Heart Association Guidelines. Anyway, that's enough of a rant. Enjoy the article and until next time!
ADDENDUM: Someone who follows my on instagram named Jessie just opened my eyes to a use case for this ROX index that I hadn't thought of before. It could potentially be used to help either alert or calm nurses and respiratory therapists regarding the potential decline of a patient who is on HFNC either in a step-down/PCU/intermediate unit. It could be an objective piece of data that they could provide to physicians to provide evidence that the patient needs to be transferred to the intensive care unit for intubation or that the patient is deteriorating. Wow! I feel silly that I had not thought of that myself but I'm glad she reached out and pointed it out to me. Thanks Jessie!
-EJ

Link to the Abstract
Although great care has been taken to ensure that the information in this post is accurate, eddyjoemd, LLC shall not be held responsible or in any way liable for the continued accuracy of the information, or for any errors, omissions or inaccuracies, or for any consequences arising therefrom.